William’s CDH Story
Justin and I (Stephanie) were so excited when we learned we would be parents in June 2020. I am an older mom, so we decided to do the NIPT test (blood testing) for any genetic issues and gender. So, when that came back normal, and we were having a boy, we were relieved and excited!! We assumed we were in the clear and decided to name him William! However, when we did the baby’s 20-week anatomy scan, they couldn’t find William’s stomach, and we thought that it was just positioning, so we decided to redo the exam in a couple of days. My husband Justin came to the first scan, but since we were not concerned, he didn’t come to the second one. When they saw his heart was pushed too far to the left, they realized they had found a severe defect in the diaphragm. They told me to call my husband, and I should get an amnio. That’s when panic set in. I was dumbfounded since the NIPT came back normal. After several rounds of scans and fetal MRIs, William was diagnosed with right-sided CDH, type C. At that point, we transferred care to the fetal center at Children’s Memorial Hermann Hospital.
Fortunately, we lived near Houston, so traveling to a hospital in the same city wasn’t difficult. Since his heart was pushed so far to the left, they decided to check his heart. On fetal echocardiogram, they detected a heart defect called Tetralogy of Fallot (TOF), a congenital heart condition consisting of four related heart defects that commonly occur together. CDH and TOF are both very serious conditions by themselves, but when presenting together, the conditions make William a very critical patient. We did the NIPT, an amniocentesis, and whole exome sequencing, but all genetic results returned negative for any issues. We were told that the chances of this happening with both CDH and TOF with no genetic markers was like getting struck by lightning twice. This entire situation was devastating for me.
We were so scared, confused, and very emotional. The survival rates doctors gave us were all across the board, anywhere from 20% to 40% survival. That being said, the doctors we met with were all SUPER optimistic, and that positivity kept our heads above water. I tried to maintain a normal pregnancy by building the nursery and having a baby shower– as if I were willing the best outcomes into existence through sheer force of will. My husband was convinced that we would be the family that defies all odds and breaks records! After 36 hours of labor, William started to go into distress, so we decided on a c-section. On February 9, 2021, we welcomed our son, Mr. William Frank. He was born at only 4 pounds and 13 ounces at 39 weeks gestation. Just like they warned us, he wasn’t crying, and he was very blue, and it was very hard to watch! They let me see him in the transport crib for about 30 seconds, and then the nurses swooped him away to the NICU. Because of the c-section, I couldn’t visit until the following day.
He was born surprisingly stable! He was hooked up to a ventilator, and he had so much hair. They let us give him his first bath and spend as much time as I could with him. Dr Harting’s team successfully repaired his CDH on day two after his birth. I got to hold him for the first time at four days old, and he was off the ventilator on day six. Unfortunately, the great Texas freeze of 2021 that shut down the whole state kept us from him between days five and eight. I could not call the hospital because the cell towers were down, and the lack of power or Wi-Fi hindered us from communicating. As you can imagine, I was a huge ball of stress during that time!
After a number of ups and downs in the NICU, William finally smiled and played with me. That same day, Dr. Greenleaf, William’s Cardio surgeon, told me they were going to have his first open heart surgery to repair his TOF the next day! We had battled some infections, including pneumonia. After two canceled open heart surgeries and several bronchoscopies later, we are finally having surgery! We have sent him off to surgery, said goodbye to him and all his NICU staff, cries and hugs, just to have him come back to the NICU with pneumonia. On April 23, 2021, when William was two months old, William had open heart surgery to repair a combination of heart defects, primarily pulmonary artery narrowing and a ventricular septal defect (an opening in the wall between the right and left ventricles). They had to replace the pulmonary conduit to his right ventricle, which he was expected to grow out of by 2-3 years old. But otherwise, the surgery was a massive success. Between these two surgeries, William spent four months in the hospital – two months in the NICU and two months in the Pediatric Heart Intensive Care Unit (CVPICU). He was a fighter through it all. Since his first open-heart procedure, William has undergone a balloon catheterization and two stents placed in his underdeveloped left pulmonary artery.
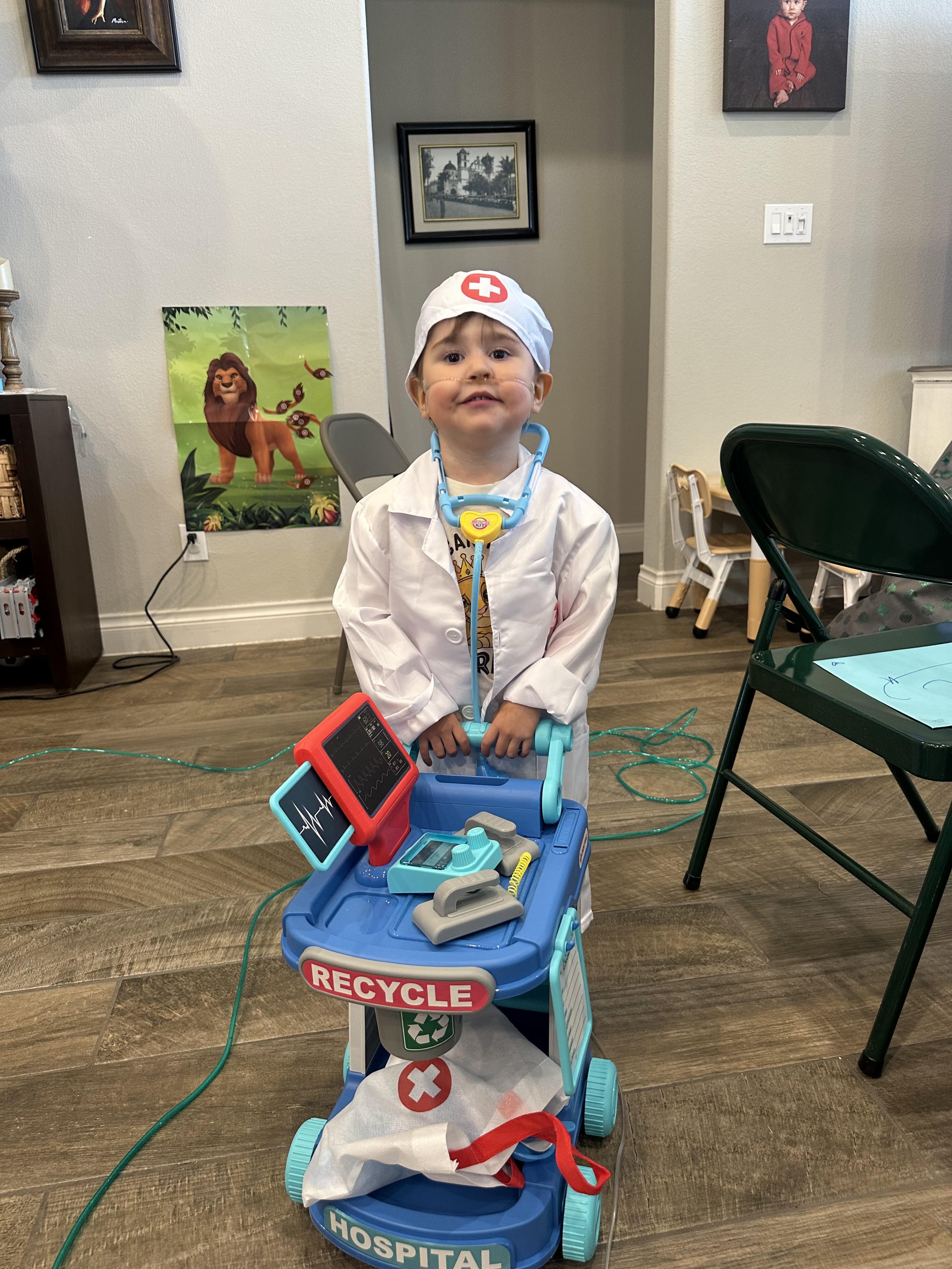
On November 30, 2023, Dr. Greenleaf performed William’s second open-heart conduit replacement, allowing adjustments to be made as he grows. They were ambitiously able to place an adult-sized stented valve, which will hopefully prevent any more open-heart surgeries. They anticipated him to be in the hospital 10-14 days post-open heart surgery. They said anything shorter is a miracle, and anything longer is a complication, but considering he’s so complex due to the CDH, we should anticipate it being closer to the 14-day mark. To everyone’s astonishment, we were in only six days. Quite the miracle! William’s recovery from this open-heart procedure has been LIFE CHANGING. He’s so much more active and hungry, and his communication skills have skyrocketed! He is a super active toddler who just turned three years old. He is happy and curious and wild! I cannot wait to see where he goes from here! We are still working to wean him off oxygen as his doctors still want to be conservative due to his persistent pulmonary hypertension and to protect the new conduit. While it was so hard to see him in the hospital hurting, he came out super strong, and I truly believe he is capable of anything!